Insights
Why are there not more Post Occupancy Evaluations in healthcare projects?
By Gemma Ham - Consultant

Overview
Why are there not more Post Occupancy Evaluations in healthcare projects?
Post Occupancy Evaluation is a term which is talked about a great deal within the healthcare construction industry and was a hot topic of discussion at the recent European Healthcare Design conference in June 2023. The concept of Post Occupancy Evaluation (POE) is not a new one and has been around since the 1960s, but is it fully embedded into the healthcare construction industry today? Whilst in theory, the evaluation of a project post completion is seen as best practice and the responsible thing to do, does this actually happen? MJ Medical have recently undertaken some research in order to investigate if POEs are common place within NHS capital projects. If not, then what are the barriers preventing POEs being completed and, if they are undertaken, are they found to be beneficial and what is done with the information gathered?
POE is a process of systematically evaluating the performance of buildings after they have been built and occupied for some time, analysing how occupants assess the built environment and obtaining feedback on a building’s performance ‘in-use’. The data gathered from a POE can be beneficial to the design team and the building owner in a number of ways, including:
- Revealing how a building is being used and identifying any inefficiencies if a building or space is not being used as intended
- Verifying if the building’s energy performance has met the expectations set out in the design stage
- Reducing operational costs by understanding the way the building is being used and its energy efficiency and identifying where efficiencies could be achieved
- Identifying if the building meets the desired functional requirements of the people who use it
- Improving decision making on future projects in terms of design and project delivery.
The benefits and value of POE are recognised by the government and the construction industry, with the inclusion of references to POE in numerous standard form project contracts, guidance and procurement frameworks. However, it is not mandatory and it does not appear that much is done to enforce this stage in the project cycle.
Research approach
In order to explore the extent to which POEs take place within the NHS post-completion of capital projects, why they might not take place, and how the information is used if they are undertaken, MJ Medical sent out Freedom of Information (FOI) requests to approximately 200 NHS Trusts asking them the following questions:
- Has the Trust completed any capital projects in the last 5 years?
- Was a POE carried out after the project’s completion?
- If no, what were the reasons for not carrying out a POE?
- If yes, did the Trust find the results of the POE beneficial?
- If yes, were the results published and/or shared within the wider NHS?
This was followed up with further discussions with some of the Trusts who responded to the FOI and a P22 contractor to find out more about their experiences of POE.
Results
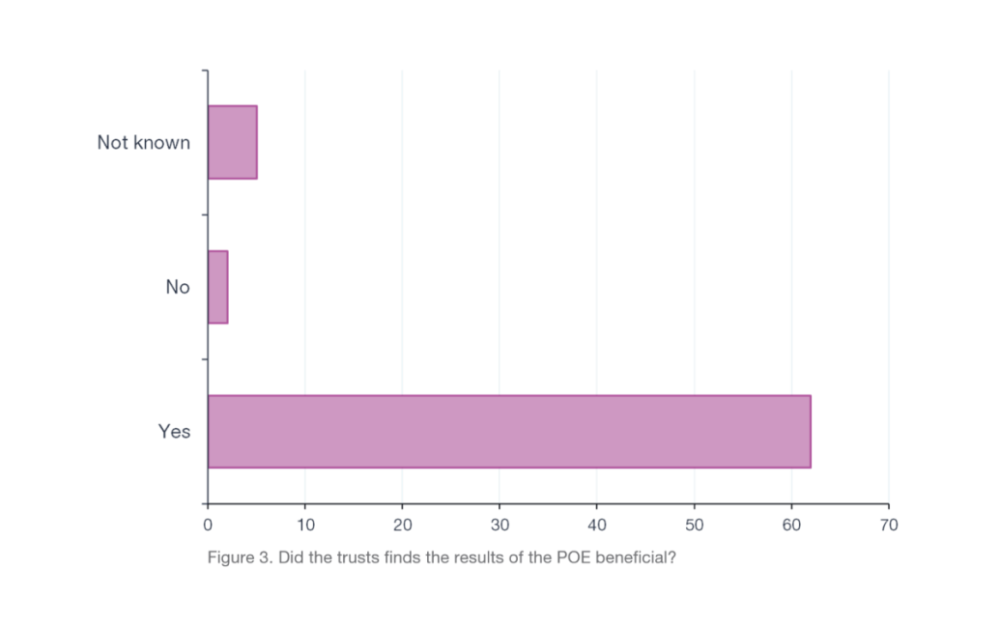
Our results showed that the majority of Trusts who responded had completed capital projects within the last 5 years, providing the potential for there to have been plenty of POEs completed (Figure 1).
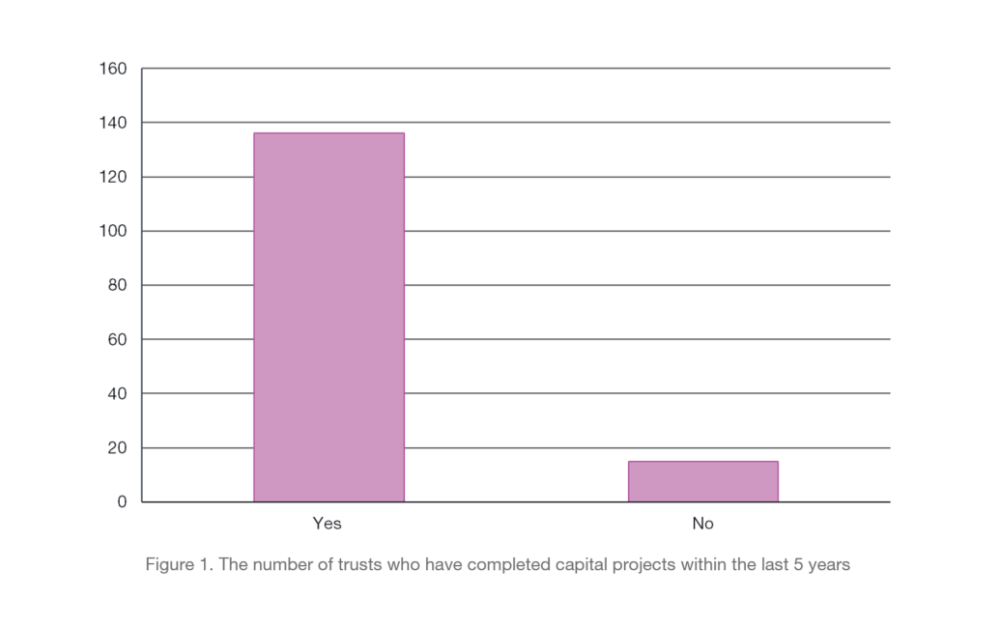
However, in response to the question about whether POEs had been completed the results were mixed. There was a fairly even split between Trusts who had undertaken a POE on their projects (41%), those who had not (49%), and a further 10% saying that they had undertaken a POE on some projects but not all. The results appear to show a real lack of consistency in the implementation of POEs (Figure 2). Further investigation into the reasons behind the ‘No’ responses identified the following common themes:
- Project size/value – Some Trusts reported that for smaller projects (such as refurbishments or office renovations), projects that were of relatively low value or that did not follow a framework such as ProCure23 or the RIBA plan of work, a POE was not deemed as required.
- COVID-19 – In looking at the past 5 years in our research the COVID-19 pandemic has obviously had an impact on normal activities. A number of Trusts had projects which finished just before the start of the pandemic meaning that the restrictions brought in during this period prevented them gaining access to staff and areas in order to carry out a POE and there was a major shift in priorities.
- Lack of resources/time – A common response was that lack of time and resources were key factors in preventing POEs taking place. With all of the pressures in the NHS it can be hard to dedicate time to a process such as a POE. Once a project has finished project teams quickly move on to the next one and other priorities take precedence. A POE is not always seen as short term project critical.
- Not part of the processes employed – A number of Trusts said that POE was simply not part of their process especially if the project was not publicly funded or part of a framework. Some Trusts did explain that they are currently reviewing their process and are looking to implement POE in the future, perhaps demonstrating that there is an understanding that undertaking POE is the right thing to do and is a valuable part of the project process. However, currently there is no set or mandated process to follow when it comes to POE therefore it is not always done or, where done, it can take various different forms with some approaches being more formal than others.
- Cost/size of the task – A POE can be a large and costly task to undertake, particularly for large new build hospital projects. One well known Trust reported in their response that they had started a POE on their new hospital but it has never been completed partly due to the size and cost of the task
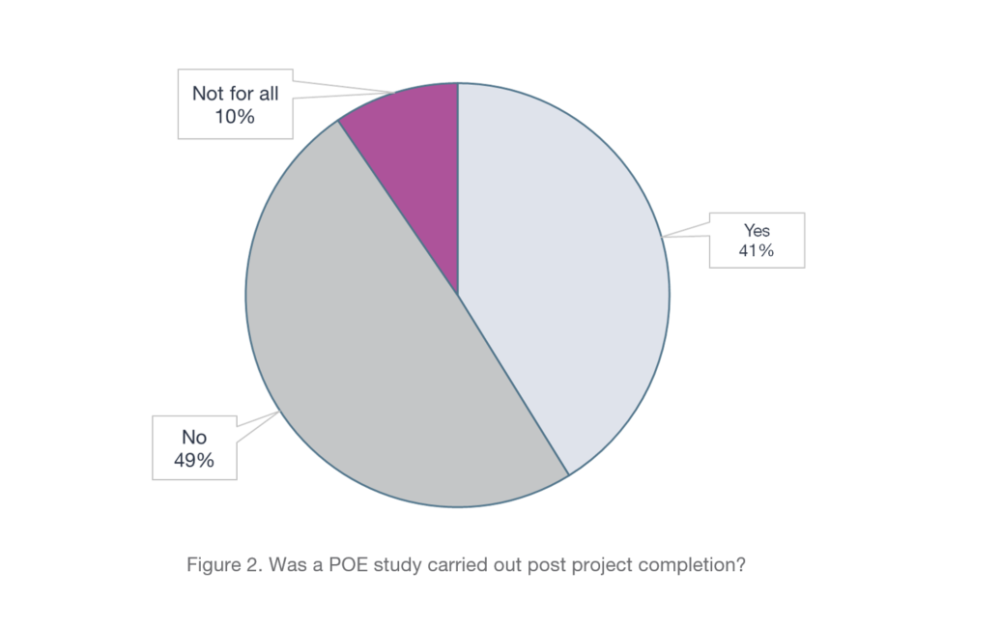
The results of our research showed that when completed, a POE is considered to be a worthwhile and informative process. Of all the Trusts who responded to the FOI and had undertaken a POE the majority had found the POE to have been of benefit and a valuable exercise with some Trusts reporting that the results from the POEs had led them to make changes and improvements to their processes and systems.
Results
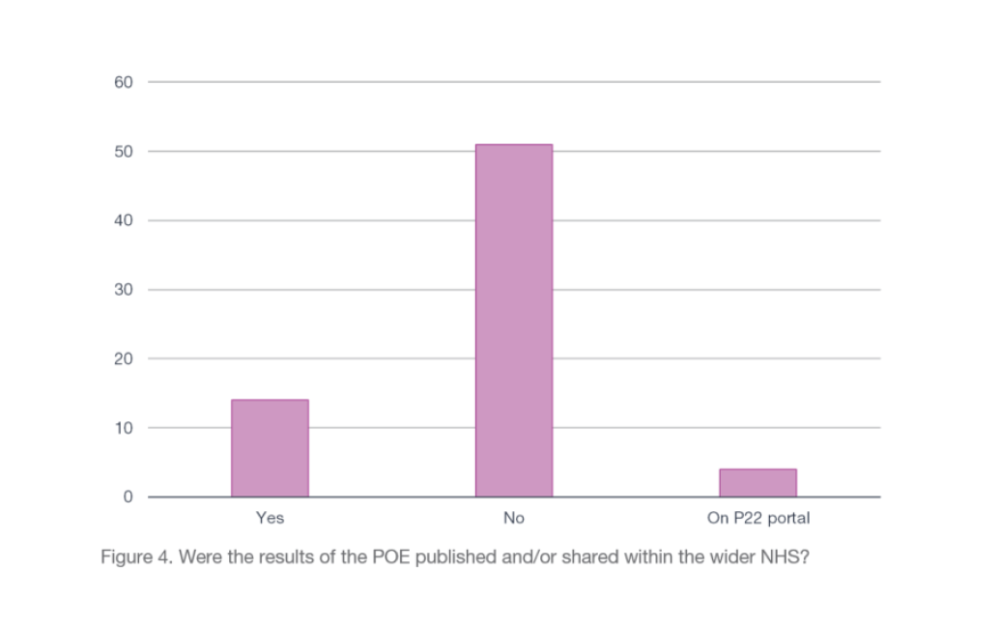
We were also interested to find out what was done with the results of POEs. In a world of more collaborative working and where the benefits of knowledge sharing are well known, are the results of POEs shared by Trusts amongst the wider NHS? The outcomes of a POE seem like the ideal type of information to be made available within the NHS, allowing Trusts undertaking a capital project to benefit from the positive experiences and lessons learned of others who may have undertaken a similar project. However, in reality it appears that this does not happen very often. The majority of respondents to the FOI who had undertaken a POE had not shared the results with the wider NHS (Figure 4).
Most Trusts reported that their POE findings were only shared internally or at the most just within their own Trust or Integrated Care Board. For projects which are completed under the ProCure framework there is a requirement for a POE to be undertaken by the contractor and shared on their portal, accessible by all the contractors on the framework, but it is not necessarily shared within the NHS. Some Trusts did say that they shared their POE results with NHSE/I and the Department of Health and Social care as part of the requirements of the project, but it was unclear what is then done with this information by these organisations.
From the results of our research it appears that it simply does not seem to be standard practice within the NHS to share this type of information, but why is this? Is it because there is a fear of exposing issues? If a project has not gone as well as expected or a building is not being used as the design intended, do Trusts want to share this with a wider audience? Further reasons for this could include; not wishing to share commercially sensitive information about suppliers which could affect future working relationships or influence others opinions on suppliers, and wishing to protect restricted information such as information on secure mental healthcare facility designs.
Conclusions
The lack of both POEs and knowledge sharing actually being undertaken in the healthcare construction industry could be seen as concerning. In a recent BBC report on the ‘Hundreds of problems found in NHS Scotland building projects’, an industry expert was quoted as saying; “One of the major issues is that there is no feedback built into the system – a new hospital is constructed but there is no review after the construction to find out what works and what does not work. Thus, there is no systematic learning between one project and the next, most of the design teams and architects will have already left site so they are none the wiser.” So, what could be done to change this culture?
More needs to be done to encourage the completion of POEs. If a POE is a contractual obligation, then more should be done to ensure both Trusts and design teams do undertake them. Introducing more processes to validate that all of the conditions of funding have been adhered to and a need to evidence that a POE has taken place as part of receiving the full funding for a project could lead to an increased uptake of the POE process. Time and resources need to be dedicated to undertaking POEs post-project completion. Whether it be a design team or an internal Trust team, ensuring that resources are made available and dedicated time for POE is programmed in is a critical part of the process and should be the norm. A standardised approach to POE could also help with an increase in implementation. A set process to follow or set of template documents made available to use could help to promote the use of POE, making it feel less of a daunting task to carry out or that a particular skill set is required. Standardised documentation could also help with the sharing and comparison of findings.
Undertaking more POEs and sharing this information would also help to inform evidence based design. In an industry that focuses very much on evidence and best practice, information gathered via the POE process should be considered essential to the successful design and delivery of future projects throughout the NHS. Sharing successes and lessons learned for similar projects could help to develop best practice in specific and patient sensitive building typologies, such as cancer care or children’s hospitals. Likewise, sharing findings from POEs on environmental measures to a wider audience could help Trusts to work together collaboratively to achieve NHS net zero carbon ambitions.
Our research has shown that POEs, a valuable and worthwhile part of the healthcare facility development process, are often overlooked. Without these reviews we cannot learn what has worked well and what has not, meaning design issues could remain undetected and could lead to them being repeated in future projects. Given recent examples of significant shortcomings in design and performance of recently completed major healthcare buildings in the UK, the cost-benefit case for POEs is clear. The time may have come for considering mandating POEs, and sharing their findings publicly, within the NHS capital development process.